TAP Block Pain Evaluation
WHERE are you hurting???
It is critically important that you evaluate closely the location (and quality) of your patient’s pain before recommending changes in therapy or deciding whether your TAP or Subcostal TAP block is functioning properly. Without proper evaluation (and elucidating in the chart or face to face), your block may be considered a failure, seen as a waste of money or could even lead to worse outcomes. Beyond these, if you can’t figure out what is going on, you will certainly not be able to optimize your patient care goals. It is critical to your ability to expand your nerve block program, especially early on, that you be able to understand the subtleties of pain evaluation and what your blocks cover (& what they do not cover). In addition, this will help you to select the most appropriate location of your TAP block placement from the start!
Let’s talk about this in reference to the TAP block. I have done hundreds of TAP blocks for abdominal surgery and found the visceral pain element to be minimal or non-existent. This is especially true in colon resections as the bowels are not stretching at all due to the initial surgically-induced ileus. Many patients go without opioids at all throughout their hospitalization, ambulate early and get return of bowel function quickly. Therefore, this is not a debate of whether this is an adequate or optimal decision or not; this is a discussion of how to optimize this therapy.
First, do not accept vague descriptions from your patient about where they are hurting. The turned away head and waving hand somewhere over the abdomen are completely useless. Tell them to use one finger to point to the area that hurts. You want to find out if that is at baseline or only with P.T. and/or coughing. Determining the quality of their sensation without leading them into one thing or another is another important skill. We’ll discuss more about obtaining a good pain history in future posts.
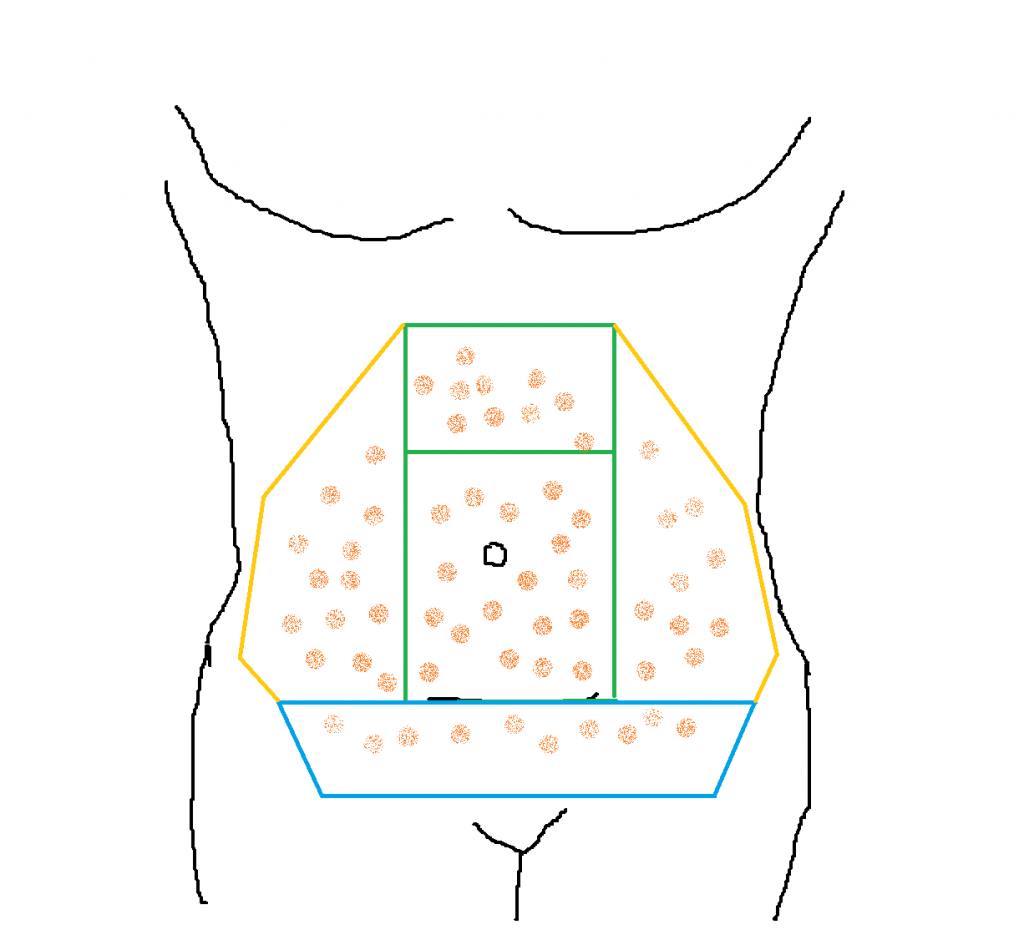
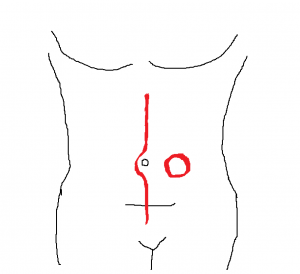
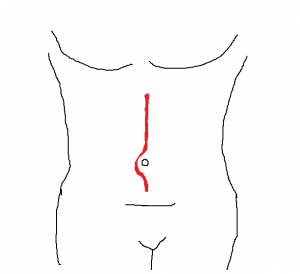
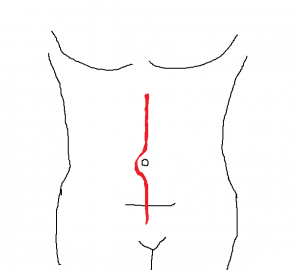
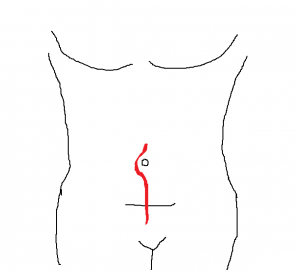
I break down the regions that you should evaluate in the above drawing. You should use an objective tool to determine surface sensation and/or temperature discrimination as well as the patient’s report of location of pain.[wlm_nonmember]
REGISTER for FREE to become a SUBSCRIBER or LOGIN HERE to view the full article!
[/wlm_nonmember]
[wlm_ismember]
The various colored blocks indicate separate regions that are covered by separate nerve paths. The two green blocks represent the distribution of coverage for a Rectus Sheath Nerve Block or a TAP Block that is performed just lateral to the appearance of the three muscle layers (External Oblique, Internal Oblique and Transverse Abdominus). That is, the lateral cutaneous branches are not covered. The coverage to the top of a full exploratory laparotomy incision, the area of the upper green box, is very variable with a TAP block, but I have seen it successfully cover the top of this incision. I will almost always select a Subcostal TAP for this incision myself. You should see how high the decreased temperature sensation goes on the abdomen and see if that goes along with the patient’s complaint of pain (ie, it only hurts at the top or the very bottom of the incision). Bolusing the catheters and/or increasing the rate of infusion may help here. Make note that the nerves come around the body heading in a slightly caudal direction, not straight across the abdomen. Consider this when approaching the area to be covered by your TAP block. Make certain that you evaluate temperature discrimination medial enough so that you don’t come to think your block isn’t working because you simply missed only the lateral cutaneous branches. Check, as well, the lateral distribution of decreased temperature sensation to see if you did also get the lateral cutaneous branch.
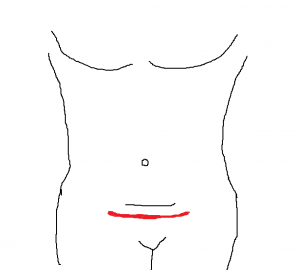
This brings me to the next point. For incisions beyond the midline, you must perform the TAP block lateral enough to get the lateral cutaneous branches. As well, bolusing may spread your local anesthetic ‘puddle’ further laterally to catch this branch before it breaks off. When performing a TAP block, it is important to move laterally whenever feasible whenever there is an incision (or colostomy) that will require this lateral distribution. Obviously, you only need to move laterally on the side where the colostomy was/will be performed. I have had patients on rare occasion with only spots of pain at the lateral edges of Pfannenstiel incisions that improved with catheter boluses.
Pain that is felt at the most caudal end of a midline incision, as mentioned above, may just need to spread a little further caudally, but it may be that it is not covering the Ilioinguinal/Iliohypogastric (II/IH) Nerves. Sensation that abruptly returns just below ‘the spare tire’ likely means that the II/IH Nerves were missed. Note whether this distinct change is bilateral or not. Again, the solution may lie in a further bolus to spread to the II/IH Nerves. It is important to identify the position of the II/IH Nerves when performing a TAP block if the surgical incision extends to the inguinal region. They will be encountered more laterally, the higher you go toward the axilla. Conversely, they are more medial as you move caudally.
The orange spots on the drawing at the top of the screen represent the cramping and diffuse nature of visceral pain that will not be covered by this abdominal wall block. Recognizing an intermittent, diffuse and cramping sensation will help you determine that bolusing your catheters will not be of use here. Again, I have hardly ever found this to be of consequence for the range of abdominal cases that I have used TAP and Subcostal TAP blocks to cover, but you should be able to identify this in order to optimize treatment.
[/wlm_ismember]
I hope this was helpful and will be on your mind the next time you consider doing a TAP block or are following-up on your patients the following days! Consider your plan for TAP blocks for the following incisions: