INFRACLAVICULAR
As I have mentioned in other places on this website, I have traditionally been more of a supraclavicular than an infraclavicular block fan. A recent conversation (rather, a friendly argument) gave me enough pause to look again at this technique. I will cut to the chase and say that I still have no good reason to alter my current regular practice of using supraclavicular catheters. Although there are ways to overcome the coracoid process getting in the way (abduct the arm, flexed at the elbow), I still find that vessels interfere with my needle trajectory every bit as much as any stray vessel does with the supraclavicular approach. I will say, however, that when a patient has the clustered arrangement of the divisions passing too far over the subclavian artery (toward the 1 o’ clock position or further medially) or spread over a ‘greater than normal’ area, I may look to change my approach to infraclavicular in this situation. The ‘corner pocket’ may be less reliable in the scenarios am describing for the supraclavicular approach, and if it doesn’t look like there is a reasonable position somewhere within the plexus, the infraclavicular will be my go-to block. Keep in mind, however, that the that the axillary nerve branches early from the posterior cord and innervates the most proximal aspect of the humerus. The infraclavicular block may be unreliable for surgery above the elbow in a minority of patients. More commonly mentioned, the musculocutaneous nerve also separates away from the cords (as the ‘upper’ part of the ‘M’) to dive into the biceps and could be missed with an approach that is too distal.
So, after properly qualifying my position, let me mention some of the positive qualities of the infraclavicular approach. First, the sonoanatomy is very simple: 2 vascular structures beneath two stacked muscle bellies and three bright spots on either side and below the axillary artery. Don’t be fooled into thinking that the bright spot under the artery is definitely the posterior cord (but ultimately, the exact position of the posterior cord as you begin the injection is irrelevant). This position behind the artery can be posterior acoustic enhancement. There aren’t a lot of other other things that are necessary to clarify in this region except for the lung which should stand out pretty clearly, and there is no need to ‘track along’ to watch for necessary changes to let you know you are in the right position. The only caveat here is the point I made above where the deltoid branch of the thoracoacromial artery or cephalic vein can be in the way. Actually, tracking a short distance is worthwhile to search for these vessels and sometimes helps to determine the position where the cords may be seen more sharply. In addition, you should look for these vessels as you would in any location (pause to look for arterial pulsation, relieve pressure to look for compressed veins, color-flow if you are not confident). As with the supraclavicular block, usually a slight movement with your fingers should identify an unobstructed needle path.
Another advantage of this nerve block is the security of the catheter. This has been mentioned many times throughout the literature and is one of the reasons it is initially selected over the supraclavicular approach. See the supraclavicular section for all the reasons why I say this is a non-factor. The three cords are in relative close proximity, so the catheter should be able to easily diffuse to all three targets. You should make yourself aware of whether you are using an open-ended catheter or closed tip (multi-orifice) catheter when you decide where to optimally place it, however. If you only insert the end of the catheter to the edge of the artery (say the 7 o’ clock position) where you inject your local anesthetic, much of your infusion will be distributed at a distance from your target with a multi-orifice catheter. It is the same case with some other sites. It should also be mentioned that there is essentially zero chance of hemi-diaphragmatic palsy from this block as compared with the interscalene and even supraclavicular blocks.
The above cadaver picture of the left neck and shoulder shows an overview of the arrangement of the brachial plexus with a needle in place for an infraclavicular nerve block. The clavicle has been removed and can be seen just behind the needle. For reference, the coracoid process can be seen as a dull yellow spot in the upper right right part of the picture with white bands (tendons of short head of biceps and coracobrachialis muscles) extending toward the right lower corner of the picture. Remnants of the cephalic vein and deltoid branch of the thoracoacromial artery are seen crossing anterior to the brachial plexus and are pushed just behind the needle. Part of the rib cage can has been cut away, and the lung is seen beneath it. You can see that the plexus is actually quite some distance from the lung (especially as you move laterally) and that abducting the arm away from the chest will move the plexus farther away. Flexing the elbow and placing the wrist at head level will also bring the plexus closer to the surface. The ‘M’ shape of the distal plexus can be seen just past the needle surrounding the axillary artery. From top to bottom, the ‘M’ is the musculocutaneous nerve, the median nerve and the ulnar nerve. Where the axillary artery is seen emerging from behind where the nerves are splitting is the split of the musculocutaneous (above artery and going toward the biceps to the right) from the portion of the lateral cord that joins a portion of the medial cord to form the median nerve. If you follow this nerve portion distally, you will see it join the medial portion to form the median nerve. This should orient you to the medial cord as well as to the ulnar nerve that leaves it as well. The radial nerve is seen coming out from behind the axillary artery. The following picture illustrates the ‘M’ further by identifying the median nerve, the middle part of the ‘M’. The next picture identifies the median nerve with contributions from the medial and lateral cord. The tip of the instrument touches the axillary artery, and the posterior cord is at the tip of it. The axillary vein is seen just below the ulnar nerve and sitting over the rib cage.
Here are a few points on optimizing the infraclavicular nerve block further. First, scan up and down the axillary artery (pause, decompress, color-flow if needed) to find a site where there are no vessels in your way. Slightly tilting the cephalad end of the linear probe (if you have the short curvilinear probe, you are more fortunate than myself) medially will give you a more ‘end-on’ (short-axis) view of the artery and cords which should make their borders more distinct. Look at the pictures above to see the angle the artery and nerves actually take as they extend beyond the clavicle. Again, this block is going to be 3-5 cm deep, and you will be taking a relatively steep path, so you should be confident in following a ‘needle shadow’ for bigger patients. Turning the bevel of a Tuohy needle upward will help it stand out. A ‘Beam Steer’ function or digging the caudal end of the probe deeper into the patient’s chest can be helpful here as well with needle visualization. Adjust your depth to make sure you can see the pleura deep to these structures so that you can be confident that it is not just below your field of vision. I have not yet attempted the supraclavicular approach to the infraclavicular block as described by Stuart Grant at Duke. When I do, I will pass on my observations in a ‘Tips and Tricks’ down the road.
My technique is to advance the needle in plane to a point at the edge of the axillary artery below the lateral cord. When my local is injected, I want to see the lateral and posterior cord peel away from the artery. The medial cord should do the same eventually, ultimately forming a ‘U’ shape with the local anesthetic. Make needle adjustments to create this effect as needed. If this pattern of spread does not occur, expect a failed block. I aim at the juncture of the artery and posterior cord in an effort to enter this neurovascular bundle when it is necessary to continue to penetrate tissue to allow me to enter the sheath. It is disconcerting to know you are not quite within the sheath and then to try to advance your needle directly at an artery. This trick allows you to push further, knowing that if you suddenly push through, you will be between the artery and the nerve and not piercing either vital structure. Of course, being this close to an artery, make sure (as always) that you do see some dark pool of local anesthetic appearing SOMEWHERE! (A ‘swirl’ effect seen IN the artery is your cue to get some midazolam out to combat the impending neurologic symptoms! PS ALWAYS inject in small doses and aspirate before every bolus with all your blocks!) As described above, I advance my multi-orifice catheter beyond the needle until it is past the artery and posterior cord so the ports are within the neurovascular bundle. Some describe moving to each cord, but that just takes longer and increases the likelihood of vascular puncture in my opinion. Just get the the junction of the artery between the lateral and suspected posterior cord, and make minor adjustments until you have the proper spread. I find it ergonomically easier to have the patient in sitting up about 30 degrees, resting my needle hand on the patient above the clavicle. A more medial approach may be more shallow, but the clavicle will still limit your ability to enter at shallow angle, and the pleura will be closer to your target. This can be recognized in the cadaver picture above where the dome-shape made by the ribs is seen further away from the plexus as you move distally.
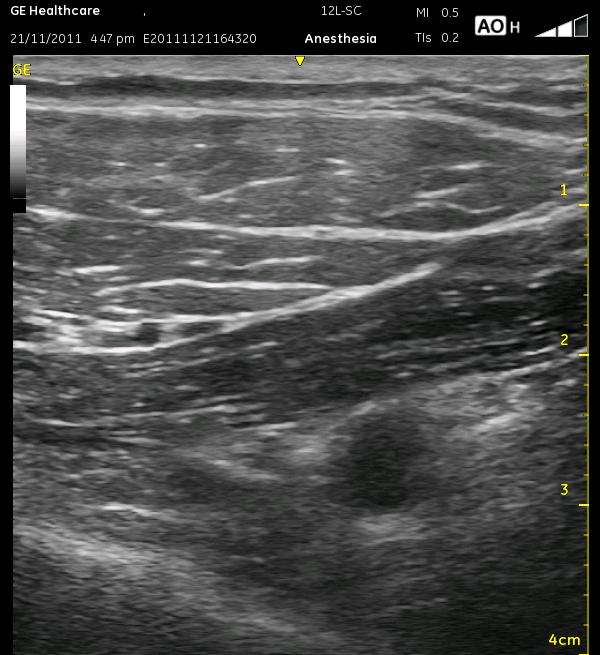
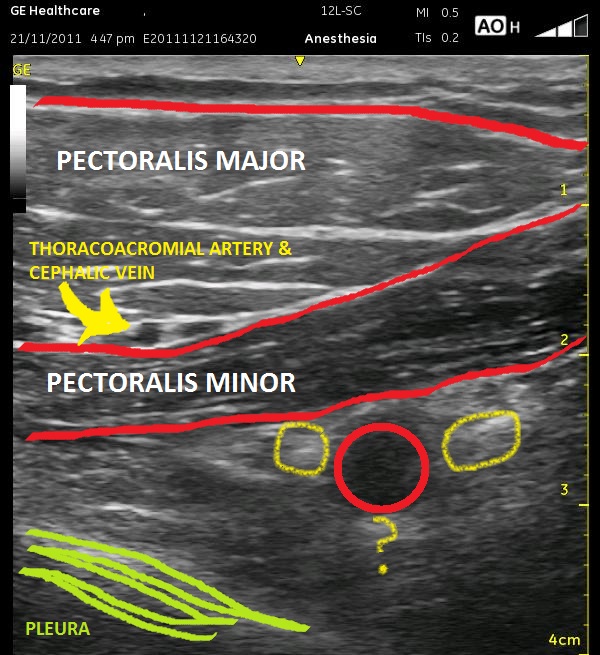
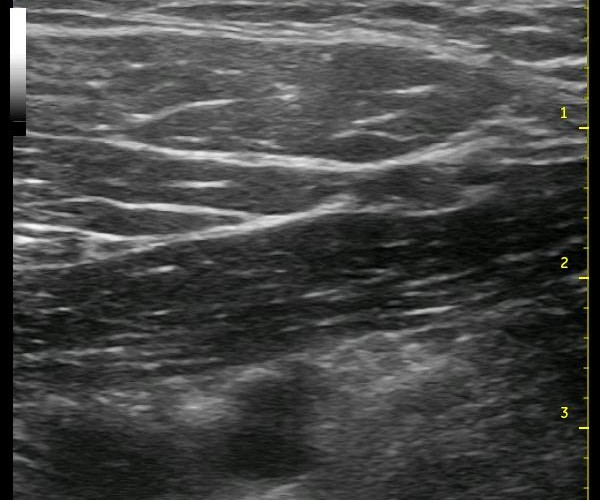
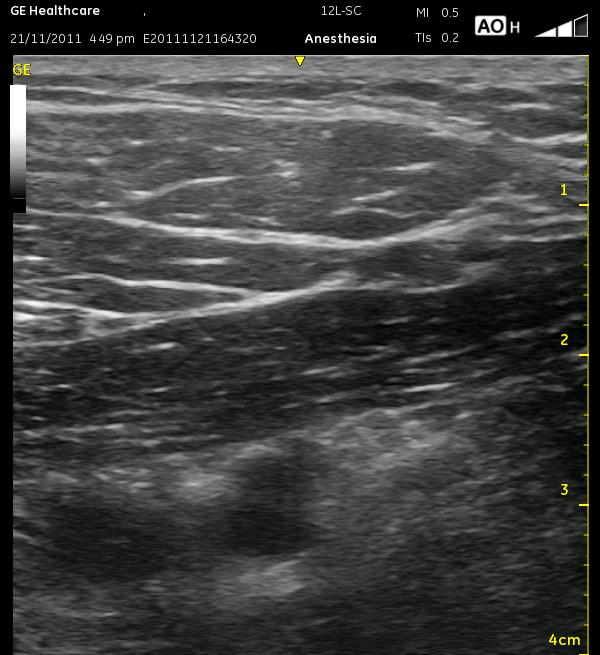
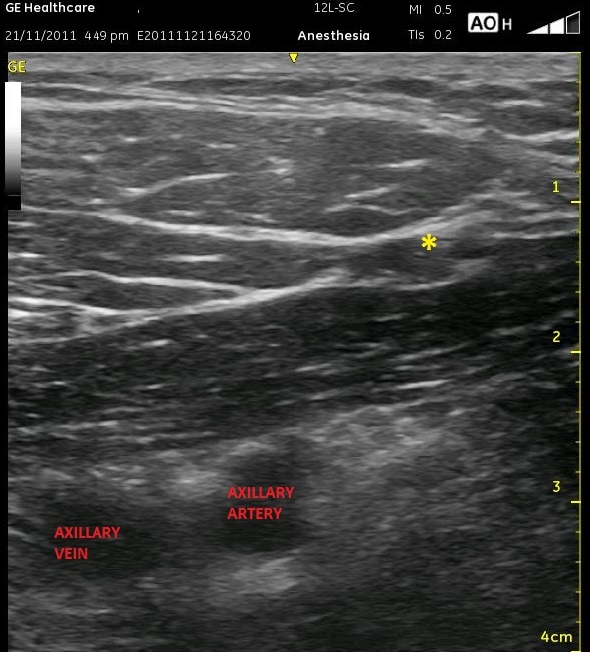
The above ultrasound pictures (cephalad is right) displays the axillary artery below the two layers of pectoral muscles. The muscle fibers are not in alignment, so the echotexture is slightly different. The pectoralis minor muscle appears slightly darker. Also, you can see the two vessel mentioned above to the left of the screen, traveling between these two muscle layers. Though it is more important in the various Pectoralis blocks, they can still help to differentiate the muscles from each other here. Either way, you should search for them as they can be easily compressed. The vessels are not in the way of the needle path as labelled, but look below at the final two ultrasound images below, and you will see that there is an artery that appears to the far right of the image. The artery can be tracked in additional images and positively confirmed.
The general locations of the cords are seen as light patches, and the axillary vein is somewhat compressed to the left of the artery. It is better visualized in the next image. The thick white edge of the pleura can be seen in the lower left corner. The artery should be moved to the left of the screen, and the needle will enter from the right, ultimately at a rather steep angle. Realize that at a steep angle, you may see only the shadow of the needle, not the needle itself. Start by aiming at closer to a 45 degree angle toward the lateral cord so the needle is better visualized, then dive at a steeper angle once you reach it. This ‘joy-sticking’ is much easier to accomplish with a larger gauge needle. Remember, using ultrasound, you can inject an ml or two to see whether you are properly in position yet or if you need to advance your needle further. Remember that the catheter should be advanced a centimeter or so beyond the needle tip. The following images display the relative position of the axillary vein during ‘decompression. The small artery as mentioned above is seen to the right of the asterisk.
The following video demonstrates what can be one of the most frustrating aspects of this nerve block approach to me. In this video, you can see very well the origins of the various branches of the thoracoacrmial artery as it branches from the axillary artery. Finding a safe trajectory in some patients can be difficult with this nerve block.