Warning: “It’s too hard to inject!”
What about HIGH Injection Pressures?
Accidental intraneural or intrafascicular injection, especially under high pressure (>15-20 psi), can lead to permanent nerve injury. Whenever we hear an experienced assistant say these words, they have our attention. At times, it is anticipated, such as when we have excellent needle tip visualization and we know that we are up against (or likely within) a tissue plane. An example might be during a single injection TAP block, and you are clearly within the thick tissue plane between the internal oblique and transversus abdominus muscles. Depending on your skill level and insight, you make appropriate adjustments. If your ultrasound skills are still developing, and the confirmation of ‘likely’ proper needle position during a nerve block is due more to your nerve stimulator alerting you of some degree of contact, it is cause for immediate action. That is, withdraw your needle immediately! In any event, this message from your experienced team demands attention. What about if you never hear this warning?
What does ‘high pressure’ feel like anyway? That is a good question, and it may vary depending on what sort of tubing you are using and how big the syringe is that you are using. More concerning than making sure that an experienced assistant can recognize ‘low’ vs ‘high’ pressures is a different observation that I commonly make when evaluating practices. What I often see is an assistant that has no conception at all that high pressure is an issue in the first place. They are focused on getting the local anesthetic injected in as quickly as possible so you don’t delay the start of the case and so they can get back to other important aspects of their job! I will often see them grip the 20 or 30ml syringe with two hands and ‘white knuckle’ it in with all their might. The other ‘adaptation’ that I have seen several times is the addition of a stopcock and a smaller (usually a 10ml) syringe which will allow them to drive the local anesthetic in faster with less force required on their part. After all, who wants to spend all day injecting or leaving work with tendonitis from all that straining?
Now, when I say that the assistant has no conception, recognize that, in actuality, I am assigning blame more to the anesthesia provider for not being aware of the issue and for not educating the staff on how to properly perform the duty at hand. (Work on your own technique, but build up and educate the team around you!) If your assistant is struggling or straining to inject, they are injecting too hard! Consider the following training tool to help your assistant get a feel for how much pressure they should use when injecting.
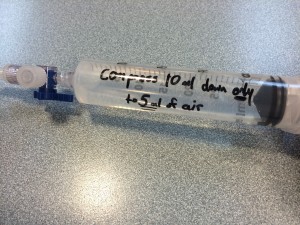
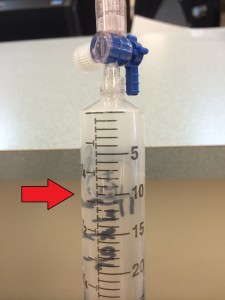
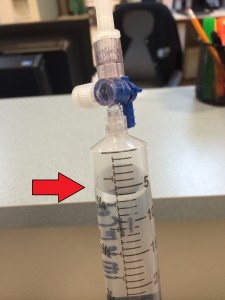
Based on Boyle’s Law, compressing a gas by 50% doubles the pressure in the system and generates about 15 psi. By adding 10ml of air and 20ml of fluid to a 30ml syringe and closing off an attached stopcock, you can recognize the maximum pressure that you should ever utilize by compressing the air from 10ml to 5ml. This can also be used during actual injections as long as your assistant directs the syringe such that the air stays within the syringe. The volume of air within the syringe should always be at least 5ml in this example.
The larger your ‘pool’ of assistants and the less experience (or greater variability of experience) they have as a whole, the greater the emphasis you must take to actively manage and monitor the seemingly minor differences in technique such as monitoring injection pressures. (Education, education, education!) Again, with a larger and more unexperienced pool of assistance, accidentally injecting air at the initiation of an injection may be more likely to occur and could be a big mess as well!
As we continue to validate the positive financial and outcomes consequences from the proper utilization of nerve blocks, these practices will continue to spread to more and more providers. We will need to continue to look for ways to allow anesthesiologists to provide these valuable services to patients more efficiently, more effectively and more safely. My belief is that pressure monitoring during nerve block injections will become a more and more important topic of discussion in the coming years.