Questions about Upper Extremity Blocks Answered
The following dialogue was generated through the CPNBconsulting.com website. This was initiated by a regional anesthesia enthusiast in Bangalore, India who had some questions for Dr Jones on upper extremity nerve blocks.
Dear Sir,
I had a few queries to clear from you:
1. Why after a supraclavicular block, are patients still be able to move
fingers and hand for almost 45 minutes through the surgery though they do
not complain of any pain?
2. Is there any possibilities of succeeding a failed block in upper
limb? I mean redo or supplement or so on
Thanks & Regards
Dr Sharanu Patil
Sparsh Hospital
Bangalore, INDIA
Dr Patil
Thank you for submitting your questions to CPNB CONSULTING! Here are my
comments on your very good questions:
1. This is more commonly seen with interscalene block from a posterior
approach because the posterior fibers at this level are primarily sensory
fibers going to the fasciculus cuneatus in the posterior columns. As well,
anterior fibers are primarily motor fibers coming from the corticospinal
tract. When local anesthetic is deposited posteriorly at the level of the
roots, there is more predominant sensory effect than motor effect. It is not
uncommon with this approach to find that the fingers never lose motor
function despite a quality sensory nerve block.
This architecture at the level of the root does not continue very far
however, and usually this effect is not maintained farther along in the
brachial plexus. That is, there is a strong sensory and motor block from
the supraclavicular and infraclavicular level block. The more likely reason
for this differential in the slower set-up of the block (if it is not
placed above the level of the first rib) is due to differences in sensory
and motor fibers themselves. Sensory fibers are much smaller and more
easily blocked than motor fibers. As well, unless you inject local at
multiple sites at the supraclavicular level (which I do not recommend),
local must travel a significant distance to thoroughly cover all of the
nerves within the plexus which can account for a slower onset of both fiber
types. A very careful physical examination might reveal that there is, in
fact, weakness in some areas of the hand and not others as the block slowly
sets up.
2. Utilizing ultrasound in experienced hands, I do believe ‘rescue’ nerve
blocks can safely be performed for failed or partial nerve blocks. I
perform ultrasound-guided continuous nerve blocks much more commonly than
single injections, so supplementing through a catheter is a safer (and would
be a more readily available) solution in this circumstance. I think the
possibility of injuring a nerve fiber with a 15 (or even 30) degree bevel
needle is greater than doing so with a Tuohy needle in a rescue block
scenario. As well, more obese patients or those circumstances where
air has been injected during the previous block (or those still in pain for
acute injuries or post-operatively with a failed nerve block) will
complicate matters, possibly reducing the level of safety when trying to
replace a nerve block.
Nerve stimulation may offer some additional safety
in this scenario; however the absence of a twitch does not imply that
nerves are not being manipulated. Blocking at a distal site
(infraclavicular or axillary) may be a better solution, especially if nerve
stimulation was planned to be used in addition. I do not recommend
replacing or supplementing a failed or partial nerve block without
ultrasound guidance.
I hope you find this information useful in your practice, and please feel
free to request further clarifications or submit more questions in the
future.
Best Regards,
Jerry Jones
CPNBconsulting.com
Dear sir,
It’s so kind of you for your prompt reply and so convincing explanation.
Will soon get back on few more things sir.
Thanks & Regards
Dr Sharanu Patil
Dr Patil
It is my pleasure, and I am glad you found this helpful. I appreciate you
granting permission to post your question on the website for the benefit of
others.
I look forward to your further inquiries.
Best regards,
Jerry Jones
CPNBconsulting.com
Dear sir,
Hope you are doing fine.
I am very fond and passionate about ultrasound nerve blocks and have been
doing it for 7 yrs. Sir, I have some queries:
1. Explanations for ulnar sparing after interscalene block
2. Routinely, when we do axillary block, the musculocutaneous(MCN) medial
cutaneous nerve of forearm and arm should get spared as MCN is not in the
same sheath as other nerves. The medial cutaneous nerves arise at cord level and above, hence they should
get spared when axillary is done. In spite of all these theories and
explanations according to many text books, we do not see any sparing as
thought to be. Sir, can you tell me a little on this?
Thanks sir
Dr Patil
 Dr Patil
Dr Patil
Thank you once again for your submission. I am always happy to hear that others are fascinated about this field!
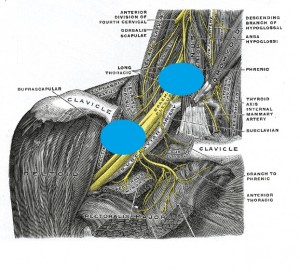
In short, when either of these nerve blocks are performed, the ‘risk’ of sparing other nerves exists due to the spatial arrangement of surrounding structures, anatomic variability and practitioner technique. If you look at my website under ‘Interscalene’, you will see a cadaver picture demonstrating that the physical distance between C5 and T1 as well as the encroaching subclavian artery CAN limit the spread of local anesthetic to the lower roots, C8 and T1. It does not mean that local WILL NOT find a path to cover these roots, it just means that it CAN happen. The suggestion is that you should consider blocking the plexus distal to the traditional interscalene target. Practically, some people are blocking, whether with nerve stimulation or ultrasound, at a point that is somewhere between the interscalene and supraclavicular position. Volume and concentration of local anesthetic can also affect the ultimate spread as well.
This circumstance also holds for the axillary and infraclavicular approach. The point here is that the musculocutaneous nerve breaks away quickly from the plexus, so infraclavicular blocks may miss it. In the axillary space, the musculocutaneous nerve ends up a distance away and within the body of the coracobrachialis muscle, so unless you are visualizing it with ultrasound, this distal technique is more likely to miss this nerve. Again, large volumes of local anesthetic and multiple needle passes and infiltrations may mean a more thoroughly covered plexus block. As well, ultrasound visualization of each of the structures will allow you to minimize the volume and the needed needle passes which grants a higher degree of safety in experienced hands.
I would be curious to know more about your approaches and techniques as well as your insights into why you do not tend to have the problem of sparing these nerves. This is certainly a benefit to your patients, and it is always good to hear questions about why problems DO NOT occur than why they ARE occurring! Thanks again for your questions!
Sincerely,
Jerry Jones
CPNBconsulting.com

