In Case of EMERGENCY, Do THIS!
One of my attendings at UT, Knoxville used to say, “If you earnestly worry about something, it won’t happen.” It was generally taken as a joke to some when it was said. It was like the ‘cure’ to a difficult arterial line insertion was having someone else open another pair of sterile gloves. It is just a superstition I guess, but the (odd to say this) sincerity in the way he always framed his comment always struck me. Worrying doesn’t stop bad things from happening, but PREPARING for (because you earnestly worry about) a disaster WILL make a difference. You will catch the disaster immediately before it escalates, and you will be fully prepared for every nuance of the presentation.
I remember the relief I had when Lipid Emulsion 20% started showing up in the literature. The worst case scenario, long-lasting cardiac arrest from LAST, was no longer a serious threat! This isn’t to say that anyone should ever be cavalier in the use of large doses of local anesthetics, but it means that there is a sure-fire rescue to this devastating outcome. Moreover, it can be used with rapidly progressing symptoms to cut short the likely eventualities which might include seizure, arrhythmia and hypotension. That is, if you are prepared, it can do all of these things!
Even in facilities that I visit where many single injections or many continuous nerve blocks are being performed, I find that there is not a ‘worst case scenario’ plan. People know that Lipid Emulsion is the answer, and they know to give…..some of it (“How many mg do you give again?”). If it is available nearby is another question. Rarely do more than one or two people know where to find it. If I ask someone to run to get it (as if something were occurring right now), they will show up again shortly with…..just a bag of lipid emulsion…..and it is still has the plastic covering around it.
If you are developing a Nerve Block Program, you need to be more ‘worried’ than this. You need to be more prepared anyway. Your team needs to be more familiar with the logistics of how to help and with what they will use to help. For example, everyone in the areas where you are performing nerve blocks and everyone on the floors where they are receiving patients with infusions should be able to ‘rapid fire’ respond with “100 ml’s” when you ask how much lipid emulsion to bolus up front. The initial bolus dose is 1.5 ml’s (not mg’s) per kg, but the answer for anyone immediately available to assist you is “100 ml’s”. What everyone around you should have on their mind is that in case of emergency, they will start drawing up two 60 ml syringes of lipid emulsion for you. With that being said, where will they get it? What else might they do while they are awaiting you? What if the patient just inadvertently pulled out their IV?

L.A.S.T. BOX
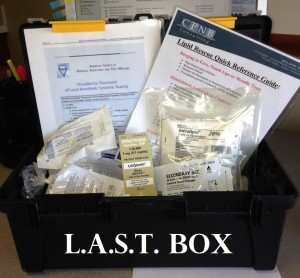
L.A.S.T. BOX
When we initiate or help to further develop a Nerve Block Program, we stage simulations to help everyone walk through the actual step-by-step processes and to familiarize them with what to do if and when the scenario changes. We also create for them a “L.A.S.T BOX”. These are easy to carry, ready to go emergency kits with essential supplies and instructions that are stationed in a number of areas throughout the facility. These L.A.S.T. BOXES are not created the same in all facilities for various reasons, but they all address the emergency needs related to the use of local anesthetic toxicity. And we tell them that we expect them NEVER to need to open the lipid emulsion! That is because of the training and preparation that should be instilled in the team. We DO expect the L.A.S.T. BOX to arrive and to be referenced for ‘what to do now’ and ‘what to start doing next’. I prefer to have them called for earlier than later, more like a Rapid Response Team than a CODE Team.

Sara Johnson RN preparing for a L.A.S.T. Simulation

Sara has a big smile for someone about to have a seizure!
I have earnestly thought through (‘worried’ about) what ought to go into these L.A.S.T BOXES, where they should be stored, and how to train the staff to use them. Maybe I should call this the ‘Bob Craft’ Box. Ha!
Have you considered the Emergency Response mechanisms for L.A.S.T. at your facility? Hopefully this gives you some good ideas!

